WELCOME TO OUR
Patient Centered Medical Home
The medical home model holds promise to improve health care in Saudi Arabia by transforming how primary care is organized and delivered. The medical home is not simply a place but rather a model of the organization of primary care that delivers the core functions of primary health care. It has remarkable similarities to the desire for Enhanced Primary Care in the new Model of Care of the National Transformation Project.
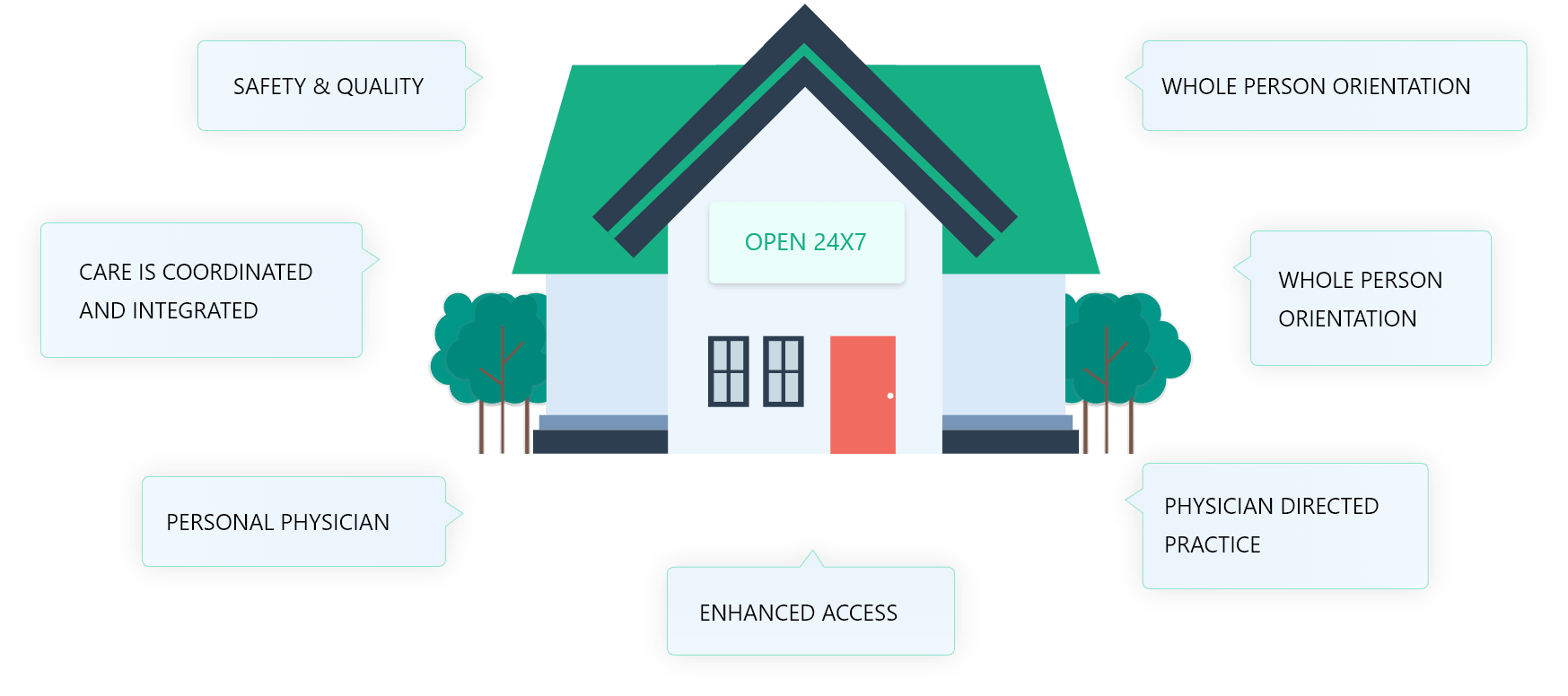
The Patient-Centered Medical Home (PCMH) is a care delivery model whereby patient treatment is coordinated through their primary care physician to ensure they receive the necessary care when and where they need it, in a manner they can understand.
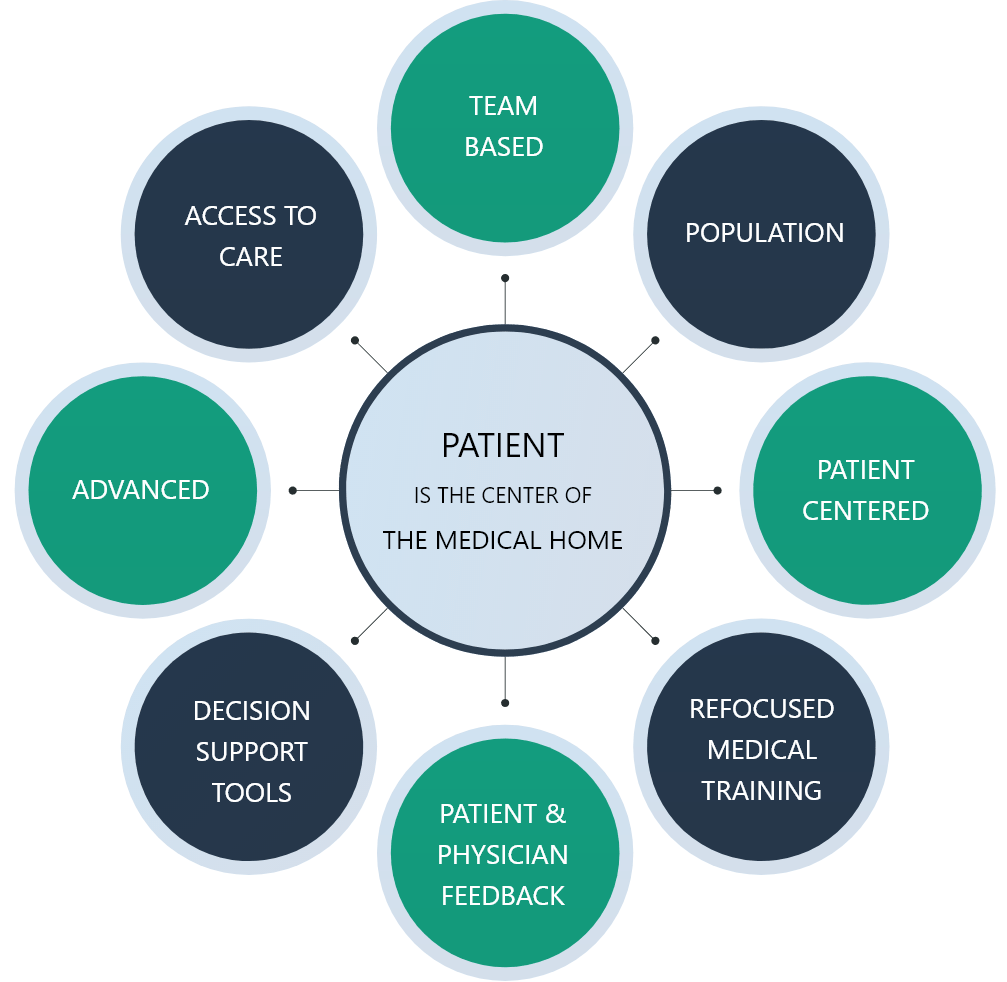
The medical home is best described as a model or philosophy of primary care that is patient-centered, comprehensive, team-based, coordinated, accessible, and focused on quality and safety. It has become a widely accepted model for how primary care should be organized and delivered throughout the health care system and is a philosophy of health care delivery that encourages providers and care teams to meet patients where they are, from the simplest to the most complex conditions. It is a place where patients are treated with respect, dignity, and compassion, and enable strong and trusting relationships with providers and staff. Above all, the medical home is not a destination instead, it is a model for achieving primary care excellence so that care is received in the right place, at the right time, and in the manner that best suits a patient's needs.

The medical home encompasses fivefunctions and attributes
Comprehensive Care
The primary care medical home is accountable for meeting the large majority of each patient’s physical and mental health care needs, including prevention and wellness, acute care, and chronic care. Providing comprehensive care requires a team of care providers. This team might include physicians, advanced practice nurses, physician assistants, nurses, pharmacists, nutritionists, social workers, educators, and care coordinators. Although some medical home practices may bring together large and diverse teams of care providers to meet the needs of their patients, many others, including smaller practices, will build virtual teams linking themselves and their patients to providers and services in their communities.
Patient-Centered
The primary care medical home provides health care that is relationship-based with an orientation toward the whole person. Partnering with patients and their families requires understanding and respecting each patient’s unique needs, culture, values, and preferences. The medical home practice actively supports patients in learning to manage and organize their own care at the level the patient chooses. Recognizing that patients and families are core members of the care team, medical home practices ensure that they are fully informed partners in establishing care plans.
Coordinated Care
The primary care medical home coordinates care across all elements of the broader health care system, including specialty care, hospitals, home health care, and community services and supports. Such coordination is particularly critical during transitions between sites of care, such as when patients are being discharged from the hospital. Medical home practices also excel at building clear and open communication among patients and families, the medical home, and members of the broader care team.
Accessible Services
The primary care medical home delivers accessible services with shorter waiting times for urgent needs, enhanced in-person hours, around-the-clock telephone or electronic access to a member of the care team, and alternative methods of communication such as email and telephone care. The medical home practice is responsive to patients’ preferences regarding access.
QUALITY AND SAFETY
The primary care medical home demonstrates a commitment to quality and quality improvement by ongoing engagement in activities such as using evidence-based medicine and clinical decision-support tools to guide shared decision making with patients and families, engaging in performance measurement and improvement, measuring and responding to patient experiences and patient satisfaction, and practicing population health management. Sharing robust quality and safety data and improvement activities publicly is also an important marker of a system-level commitment to quality.

The primary care medical home demonstrates a commitment to quality and quality improvement by ongoing engagement in activities such as using evidence-based medicine and clinical decision-support tools to guide shared decision making with patients and families, engaging in performance measurement and improvement, measuring and responding to patient experiences and patient satisfaction, and practicing population health management. Sharing robust quality and safety data and improvement activities publicly is also an important marker of a system-level commitment to quality.
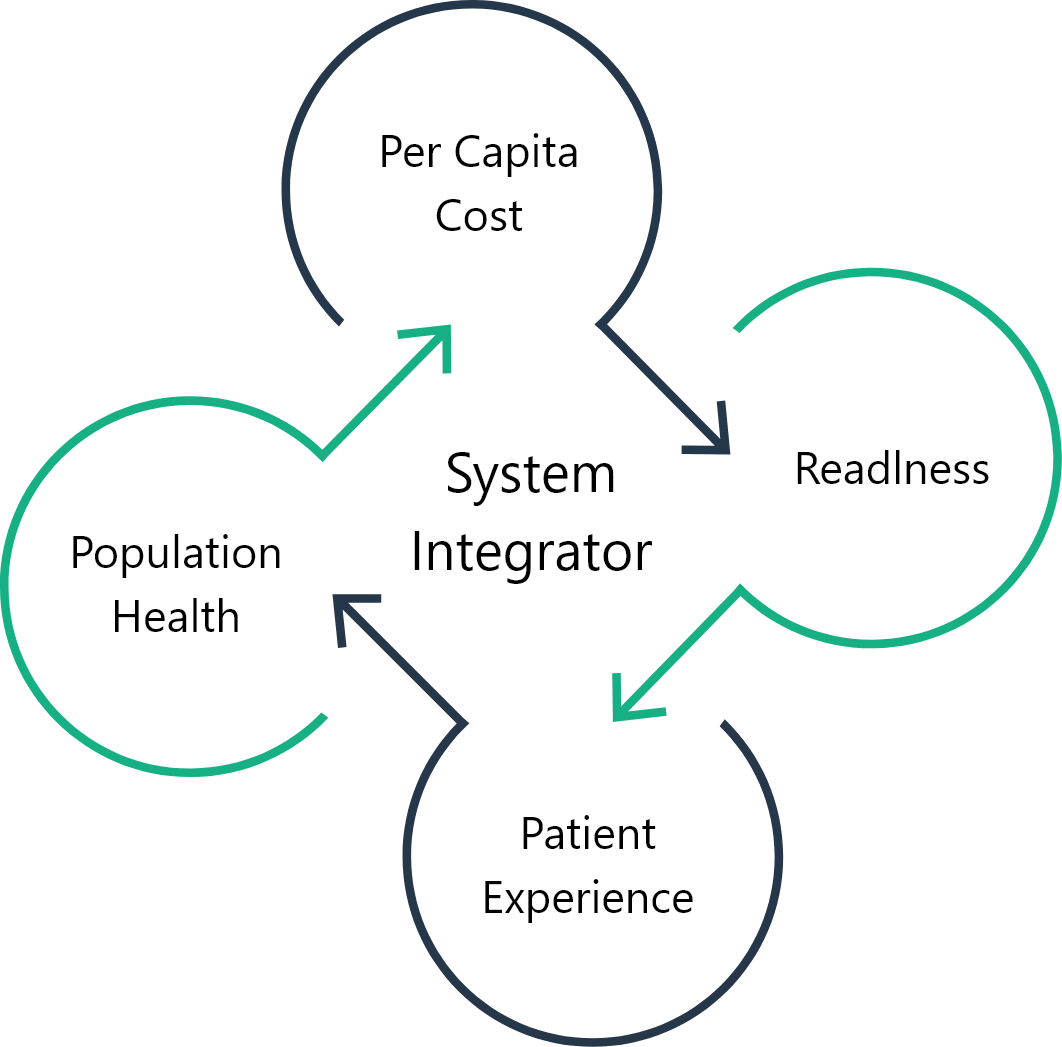
The Patient-Centered Medical Home is the ideal model of primary care to integrate with other health care organizations. There are well studied Accountable Care Organizations in the US that offer the entrance to care through the Family Medicine based PCMHs. In this way there is a accountability for care from the basic level of care to the highest tertiary care. Health Insurance companies work extensively with the PCMH. This relationship allows for smooth exchange of patient utilization data and outcomes-based data that can improve care and decrease cost. It is clear that the PCMH brings high value to the health care system, but it is also more comprehensive than stand alone primary care and hence more expensive. This is the reason that PCMH-based health systems must support the primary care systems so that they in turn can reap the dividends form improved health, less utilization and lower costs.
The medical home encompasses fivefunctions and attributes